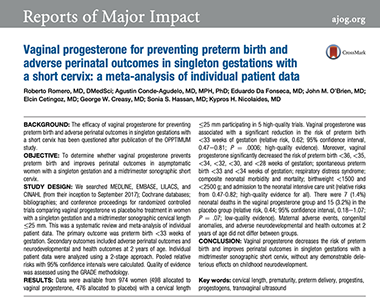
Preventing
Premature Birth

Definition of Preterm Birth
Preterm birth is defined as delivery before 37 weeks of pregnancy, or more than 3 weeks before the expected due date. Preterm birth can be classified as follows:
34-36 weeks: late preterm birth
32-34 weeks: moderately preterm birth
<32 weeks: very preterm birth
Strategies to Reduce Preterm Birth
There are three strategies that have recently been suggested to reduce the incidence of spontaneous preterm birth. The first involves screening all pregnant women, especially those having their first child. The second involves treating only those women who have had a previous preterm birth. The third describes the use of progesterone to further decrease the rate of preterm birth after premature labor has been arrested or stopped using other drugs administered in the hospital setting. The following sections will review each of these strategies.
Facts About Preterm Birth
The following are some interesting facts regarding preterm births that may be of interest to you.
1. In 2008, 1 in 8 babies (12.8% were born preterm in the United States. In 2014, 9.5% of live births were less than 37 weeks and 2.7% were less than 34 weeks
.
2. The rate of preterm birth in highest in black infants (18.1%) and lowest in Asians (10.8%).
3. Multiple births are 6 times more likely to result in preterm delivery than singletons.
4. The cost of a preterm birth is 10 times higher than a full-term birth.
5. Premature infants may face a number of health challenges that include the following:
a. Low-birth weight
b. Breathing problems because of underdeveloped lungs
c. Underdeveloped organ systems
d. Risk of life-threatening infections
e. Risk of lung disease known as respiratory distress syndrome
f. Risk of cerebral palsy
g. Risk for learning and developmental disabilities
Screening All Pregnant Women for
Preterm Birth
At the Fetal Diagnostic Center all women examined during the 2nd trimester of pregnancy are offered cervical length screening to identify whether the patient is at risk for a preterm birth. The following discusses the rationale for this evaluation and the recommended treatment when the cervix is abnormally shortened.
National Institutes of Health Study: 2011
A study funded by the National Institutes of Health published in July, 2011, reported progesterone, a naturally occurring hormone, reduced the rate of preterm birth before the 33rd week of pregnancy by 45% among women with a short cervix detected by measuring the cervical length using endovaginal ultrasound. In addition, the study also found that infants born to women who had received progesterone were less likely to develop respiratory distress syndrome (3% vs 7.6%), a breathing complication occurring in preterm infants.
458 women with a short cervix (10 to 20 millimeters) detected between 19 and 23 weeks of pregnancy, were randomly assigned to receive daily either a vaginal gel progesterone preparation or a placebo (no progesterone).
Progesterone treatment was associated with a lower rate of preterm delivery at less than 33 weeks (8.9% in the progesterone group versus 16.1% in the placebo group). Differences in the rate of preterm birth were also seen in births between 28 and 35 weeks of pregnancy. The following graph compares the premature delivery rate in patients treated with and without progesterone who had a short cervix.
Summary of Recent Studies: 2018
In 2018 Dr. Roberto Romero, Director of the Perinatal Research Branch of the National Institutes of Health reviewed all studies in which the use of vaginal progesterone was used or not used in women with a short cervix of less than 2.5 cm. They identified 498 women who received vaginal progesterone and 476 who did not receive progesterone. When comparing the two groups, vaginal progesterone decreased the risk of preterm birth and improved perinatal outcomes in singleton gestations with a mid-trimester sonographic short cervix, without any demonstrable deleterious effects on childhood neurodevelopment.
Read the Study
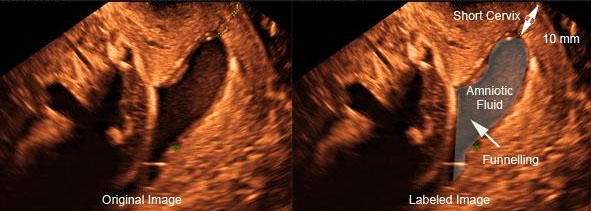
Endovaginal Ultrasound Measurement of the Cervix
Treatment: Cervical Length Between Less Than 1 Centimeter
If the cervix measures less than 1 centimeter, the risk for cervical incompetence with loss of the pregnancy is increased. Cervical incompetence results from weakness of the cervical tissue and results in early dilation of the cervix. This can be due to a number of conditions, mostly the result of prior injury to the cervix from either inherited conditions or prior cervical such as a D&C or cone biopsy.
When the cervix shortens, it dilates without contractions or pain, sometimes opening completely. The dilation results in the amniotic membranes bulging through the opening and eventually rupturing, often before the baby can survive outside of the uterus. Cervical incompetence accounts for about 15 to 20 percent of all pregnancy losses during the second trimester of pregnancy.
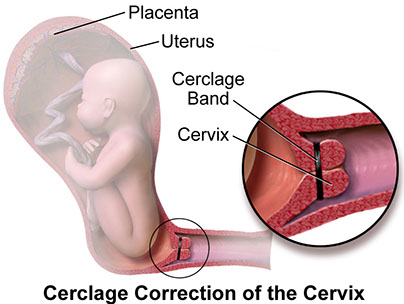
When an incompetent cervix is diagnosed, the condition may be treatable by placing a cerclage (stitching the cervix closed). If electively done because of a previous history of an incompetent cervix or other risk factors, the procedure is usually performed after the 12th week of pregnancy. If an incompetent cervix is diagnosed later in pregnancy (18-24 weeks) an emergency cerclage is often placed.
After hospital discharge, the patient may remain on bed rest in order to remove pressure on the cervix and increase the chances of retaining the pregnancy until the baby is viable. The cerclage is usually removed just before childbirth so that the patient can give birth vaginally.
From Wikepedia, Cervical Cerclage
Treatment: Cervical Length Between 1 and 2.5 Centimeters
The following are recommendations from UPTODATE, Progesterone supplementation to reduce the risk of spontaneous preterm birth
Author:Errol R Norwitz, MD, PhD, MBASection Editor:Charles J Lockwood, MD, MHCMDeputy Editor:Vanessa A Barss, MD, FACOG
"Natural or micronized progesterone — Natural progesterone is typically administered vaginally. The advantage of vaginal progesterone is its high uterine bioavailability since uterine exposure occurs before the first pass through the liver. It has few systemic side effects, but vaginal irritation can be bothersome and the drug needs to be administered daily. Doses of 90 to 400 mg have been effective, beginning as early as 18 weeks of gestation. We use 100 mg administered vaginally each evening; however, in some areas a 200 mg suppository may be more readily available and less costly. A vaginal suppository can be prepared by a compounding pharmacy utilizing a commercially available standardized kit.
Other options include a 100 mg micronized progesterone vaginal tablet or an 8 percent vaginal gel containing 90 mg micronized progesterone per dose. Both preparations are commercially available in the United States, but not approved for prevention of preterm birth in cervical shortening. The FDA concluded the data in the manufacturer's application did not sufficiently support the efficacy of progesterone 8 percent gel compared with placebo in reducing the risk of preterm births before 33 completed weeks of gestation among women with a short cervical length, but the drug was safe in this population [85]. The FDA was critical of the statistical methods used in the key trial and noted that most of the apparent treatment benefit occurred in non-United States centers.
The safety profile of vaginal progesterone in the first trimester of pregnancy is supported by extensive data from patients who received the drug for luteal support, while large trials during the second and third trimester in women at increased risk of preterm birth support its safety later in gestation.